Understanding the Flexibility of Cancer Cells
Cancer cells exhibit remarkable plasticity, adapting their characteristics as they disseminate throughout the body. Many of these adaptations stem from epigenetic modifications, which affect the packaging of DNA rather than relying solely on mutations within the DNA itself. Targeting these modifications presents challenges in cancer therapy, as they are reversible and can fluctuate between states.
Epigenetic Changes and Their Origin
Traditionally, epigenetic changes have been attributed to internal cellular mechanisms that involve the chemical tagging of DNA and histone protein packaging—for instance, processes such as histone methylation and DNA acetylation. However, a recent study led by Richard White from Ludwig Oxford and Miranda Hunter of the Memorial Sloan Kettering Cancer Center, published in the current issue of Nature, highlights the significance of the physical environment surrounding these cells as a critical factor in initiating epigenetic transformations.
Research Findings: Tumor Cell Adaptations
Utilizing a zebrafish model of melanoma, White, Hunter, and collaborators discovered that when tumor cells are confined by adjacent tissues, they undergo notable structural and functional alterations. Instead of maintaining rapid proliferation, these cells initiate a ‘neuronal invasion’ program, allowing them to migrate and infiltrate nearby tissues.
The Role of HMGB2 in Epigenetic Transformation
Central to this transformation is the protein HMGB2, which bends DNA. The study demonstrates that HMGB2 reacts to mechanical confinement by binding to chromatin. This binding modifies the packaging of genetic material, thereby exposing areas of the genome associated with invasiveness and making them available for gene expression. Consequently, cells expressing elevated levels of HMGB2 exhibit reduced proliferation but increased invasiveness and resistance to therapeutic interventions.
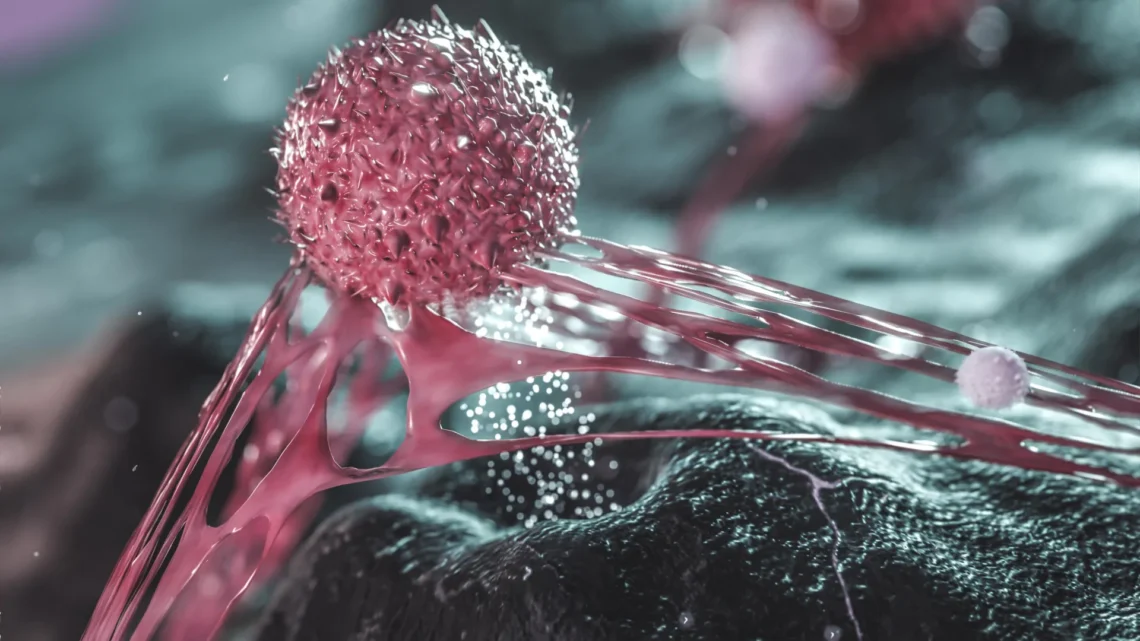
Cellular Remodeling and Protective Structures
The research team further observed that melanoma cells adapt to external mechanical pressures by restructuring their internal cytoskeletal framework, forming a cage-like formation around the nucleus. This protective structure is facilitated by the LINC complex—a molecular bridge that links the cell’s cytoskeleton to the nuclear envelope, protecting the nucleus from potential rupture and DNA damage arising from confinement-induced stress.
Implications for Cancer Treatment
“Cancer cells can rapidly switch between different states, influenced by their environmental cues,” remarked White. “Our study illustrates that mechanical forces within the tumor microenvironment can trigger these transitions. This adaptability presents significant challenges for treatment, as therapies designed to target proliferating cells may not effectively address those that have transitioned to an invasive, drug-resistant phenotype. By identifying the factors involved in this transition, we aim to develop therapies that can prevent or even reverse such invasive transformations.”
Conclusions: The Role of Tumor Microenvironment
The findings underscore the critical role of the tumor microenvironment in influencing cancer cell behavior, revealing how physical signals can prompt cells to reorganize their cytoskeleton, nucleus, and genomic architecture, resulting in a shift between growth and invasive states. Notably, this study demonstrates how physical stress can serve as a significant, yet often overlooked, driver of epigenetic changes.
Key Health Takeaway
The adaptability of cancer cells, driven by both epigenetic modifications and physical environmental factors, poses substantial challenges for treatment strategies. Understanding these dynamics may pave the way for innovative therapies that can more effectively target invasive and drug-resistant cancer phenotypes.
This study was supported by the Ludwig Institute for Cancer Research, National Cancer Institute, the Cancer Research Society, the Canadian Institutes of Health Research, the U.S. National Institutes of Health, the Melanoma Research Alliance, The Debra and Leon Black Family Foundation, the Pershing Square Sohn Foundation, The Mark Foundation, The Alan and Sandra Gerry Metastasis Research Initiative at MSKCC, The Harry J. Lloyd Foundation, Consano, the Starr Cancer Consortium and the American Cancer Society.
Richard White is a member of the Oxford Branch of the Ludwig Institute for Cancer Research and a professor of genetics at the University of Oxford, Nuffield Department of Medicine.