Mayo Clinic researchers have identified the mechanisms by which excessive alcohol consumption contributes to fatty liver disease, a condition that affects over one-third of the population in the United States. Known clinically as Metabolic Dysfunction Associated Steatotic Liver Disease, this chronic condition can lead to serious health issues, including type 2 diabetes and liver cancer. The Mayo Clinic’s recent findings shed light on the biological processes involved in this condition.
The Role of Alcohol in Fatty Liver Disease
The research team discovered that exposure to excessive alcohol alters a crucial enzyme responsible for recycling damaged proteins in liver cells.
Understanding Liver Function
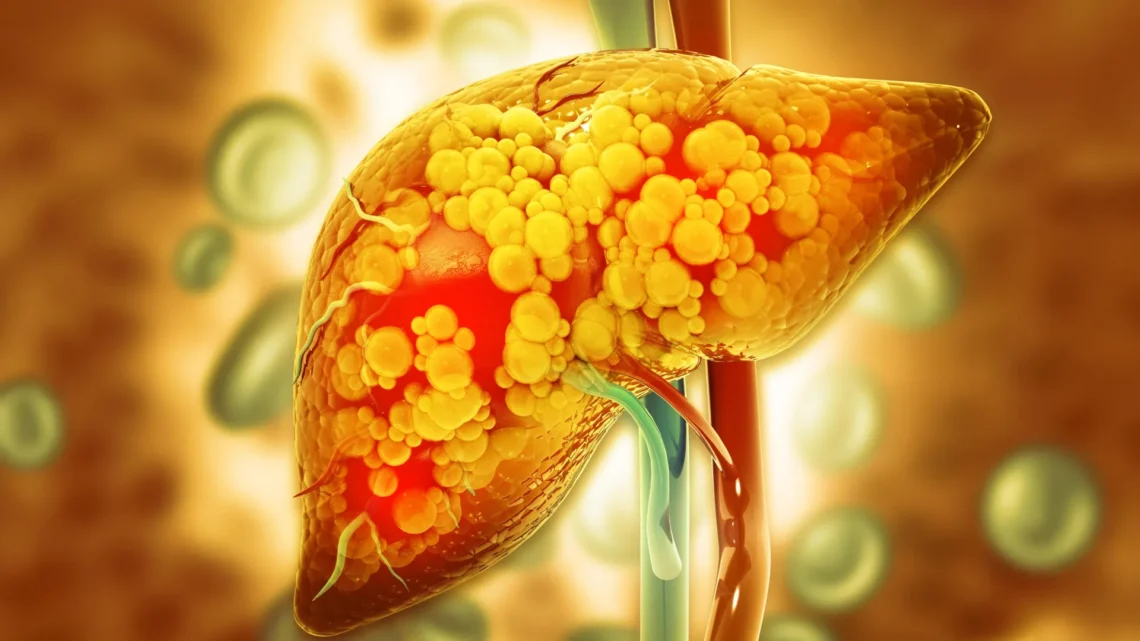
The liver serves as the primary filtration system for substances ingested by an individual. Liver cells, known as hepatocytes, perform this critical function by releasing various proteins while simultaneously collecting, sorting, degrading, and recycling nearly all materials that pass through this complex organ. For instance, fat absorbed from the gut is stored in hepatocytes as lipid droplets—globular structures that serve as reservoirs of fat for energy use during periods of fasting. Nevertheless, an overaccumulation of these lipid droplets can lead to fatty liver disease.
The Importance of Valosin-Containing Protein (VCP)
Central to this research is an enzyme known as valosin-containing protein (VCP), which plays a vital role in a multitude of cellular processes, including the recycling of unwanted proteins. In healthy individuals, VCP regulates the protein HSD17β13, preventing excessive accumulation of fat within liver cells.
“We were surprised to observe that VCP actively removes HSD17β13 from the surface of lipid droplets. When HSD17β13 accumulates, it leads to an increase in fat content in liver cells, contributing to fatty liver disease,” states Mark McNiven, Ph.D., senior author of the study published in the Journal of Cell Biology.
The Impact of Alcohol on VCP and HSD17β13
However, the research team found that excessive alcohol exposure significantly diminishes the presence of VCP on lipid droplets, allowing HSD17β13 to accumulate unchecked.
Further observations revealed the intricate recycling mechanism of VCP. The team documented VCP in collaboration with a chaperone protein to transport damaged proteins to the lysosome, an organelle responsible for breaking down unwanted proteins.
“It was remarkable to witness this process. Various experiments we conducted affirmed that VCP directs HSD17β13 from the lipid droplet to the lysosome,” explains Sandhya Sen, Ph.D., a research fellow at the Mayo Clinic and lead author of the study.
Implications for Future Therapies
The findings suggest that HSD17β13 may become a key target for developing new therapies aimed at preventing or treating fatty liver disease, according to Dr. McNiven.
“This study enhances our understanding of lipid droplet biology—the primary contributor to fatty liver disease—and the operational dynamics of hepatocytes in reducing fat content,” Dr. McNiven remarks. “Furthermore, it may help identify patients who are particularly vulnerable to the harmful effects of excessive alcohol on their liver if this cellular mechanism is compromised.”
The Precure Initiative
This research is part of the larger Precure initiative at the Mayo Clinic, which aims to create tools that enable clinicians to predict and intervene in biological processes before they escalate into diseases or progress to complex, challenging conditions.
Please refer to the study for a complete list of authors, disclosures, and funding.
Key Health Takeaway
Excessive alcohol consumption markedly influences the mechanisms regulating fat storage in the liver, emphasizing the need for awareness and intervention to prevent conditions like fatty liver disease.