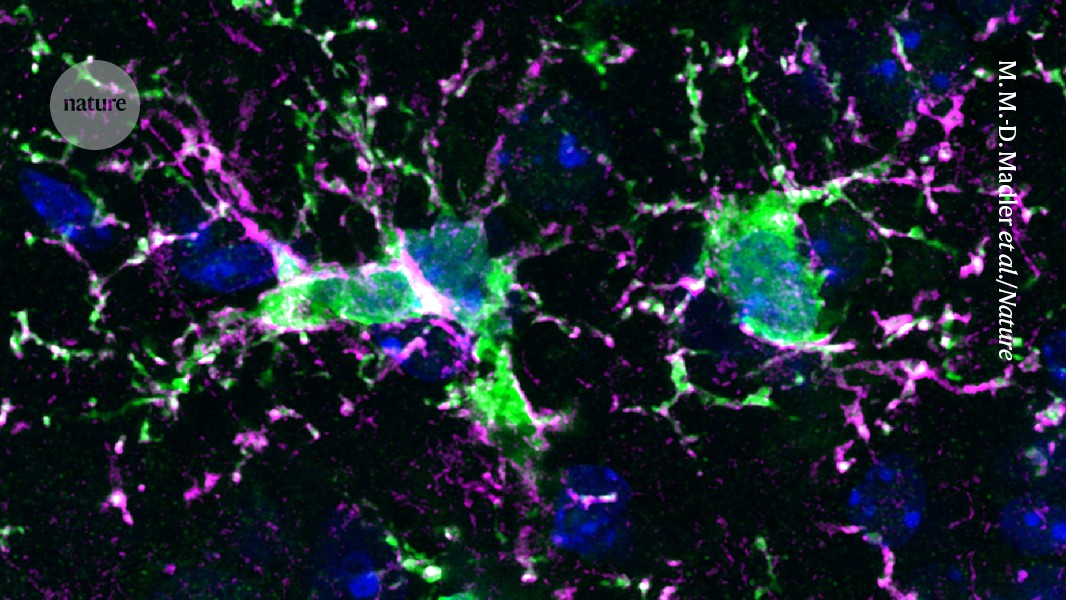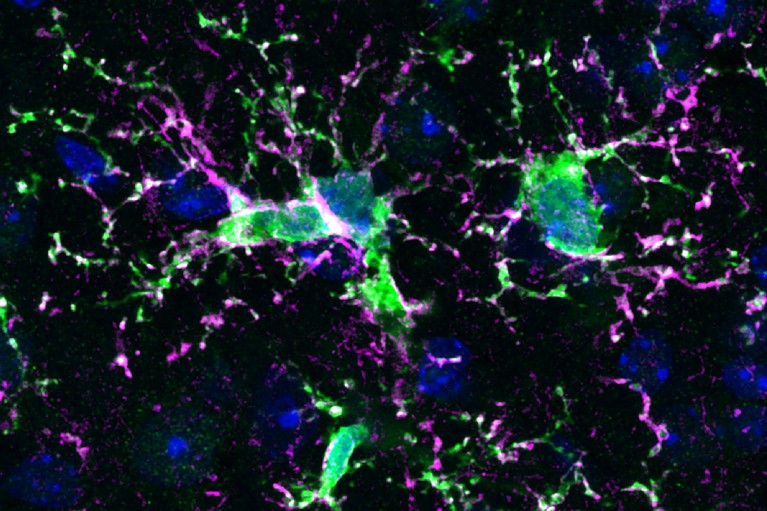
After a mouse received treatment to eliminate immune cells called microglia, it was injected with human progenitor cells that developed into human immune cells (green, pink, and blue) in the animal’s brain.
Credit: M. M.-D. Madler et al./Nature
A new approach, involving the replacement of immune cells that maintain brain health, holds promise for treating various conditions, from rare genetic disorders to more common illnesses like Alzheimer’s disease.
Recently, several studies have explored the technique known as microglia replacement, seeking to enhance its safety and efficacy. “This approach is very promising,” says Pasqualina Colella, a gene and cell therapy researcher at Stanford University School of Medicine in California. However, she adds, “the procedure can be toxic.”
New hope for Alzheimer’s: lithium supplement reverses memory loss in mice
Microglia are immune cells responsible for monitoring brain health by eliminating foreign invaders, damaged cells, and harmful substances. They play a protective role for neurons—cells that communicate information throughout the body—during conditions like seizures and strokes, while also helping to prune unnecessary neuronal connections during normal brain development.
“Microglia have a lot of critical functions,” explains Chris Bennett, a psychiatrist who studies these cells at the Children’s Hospital of Philadelphia. “It’s expected they are involved in the development of many diseases.”
Many diseases, including rare disorders caused by genetic mutations that impact microglia, as well as more well-known conditions like Alzheimer’s and Parkinson’s diseases, are associated with malfunctioning microglia, according to Bo Peng, a neuroscientist at Fudan University in Shanghai, China.
Immune-Cell Swap
Researchers are now intrigued by the possibility of treating certain brain disorders by replacing these dysfunctional microglia. However, successfully swapping microglia is notably tricky. In typical bone marrow transplants, a patient’s immune cells are refreshed by introducing stem cells from the marrow, but microglia primarily exist in the central nervous system and generate new cells through division rather than sourcing them from the marrow.
How CRISPR gene editing could help treat Alzheimer’s
Bone marrow transplants are already applied in some rare cases affecting microglia, like X-linked adrenoleukodystrophy. While these treatments show potential, Marco Prinz, a neuropathologist at the University of Freiburg, Germany, notes that results can vary and only a small fraction of the recipient’s original microglia are replaced.
In July, Peng’s research team successfully utilized bone marrow transplants to address abnormal microglia caused by a fatal brain condition known as CAMP (CSF1R-associated microgliopathy). Their approach proved effective in both mice and a small trial involving eight patients: none showed a decline in motor or cognitive functions within two years, unlike a control group who did not receive treatment.
One reason for the success of the CAMP trial might lie in the disease’s nature; patients tend to have relatively low microglia production, allowing more room for the transplanted cells to adapt.
Onerous Regimen
Creating an environment suitable for new microglia is crucial and poses a challenge. To accommodate these transplanted cells, physicians often need to first eliminate as many existing microglia as possible, which may involve high doses of chemotherapy or radiotherapy. These treatments can increase vulnerability to infections during recovery and elevate long-term cancer risks. Therefore, microglia replacement remains too risky for use outside of severe, rapidly progressing diseases like CAMP, warns Colella.
### Summary
Recent advancements in the replacement of brain immune cells known as microglia show promise for treating various neurological disorders, including Alzheimer’s. While initial studies indicate potential success, challenges remain regarding the toxicity of the procedures and the need for careful patient selection.