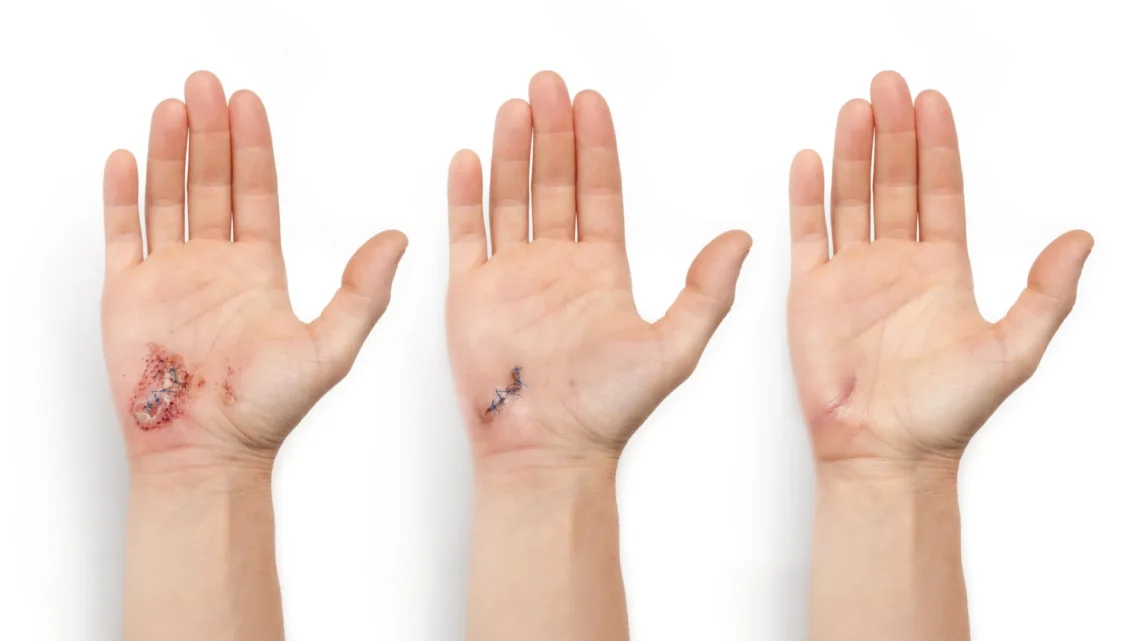
Understanding Wound Healing Stages
As a wound heals, it progresses through several stages: clotting to stop bleeding, immune system response, scabbing, and ultimately scarring.
The Development of “a-Heal”
A revolutionary wearable device known as “a-Heal,” developed by engineers at the University of California, Santa Cruz, aims to optimize each stage of the wound healing process. This innovative system employs a miniature camera and artificial intelligence (AI) to assess the healing stage and administer treatments, which can include medication or an electric field. By tailoring interventions to the individual healing process of each patient, “a-Heal” offers a personalized approach to wound care.
The portable and wireless nature of the device facilitates wound therapy for patients in remote locations or those with limited mobility. Initial preclinical results, published in the journal npj Biomedical Innovations, indicate that the device significantly accelerates the healing process.
Design and Functionality of “a-Heal”
The research team, comprised of experts from UC Santa Cruz and UC Davis, operated under the auspices of the DARPA-BETR program and is led by Marco Rolandi, the Baskin Engineering Endowed Chair and Professor of Electrical and Computer Engineering (ECE) at UC Santa Cruz. The device integrates a camera, bioelectronics, and AI to promote faster wound healing, establishing it as a “closed-loop system,” a pioneering advancement in wound care technology.
According to Rolandi, “Our system takes cues from the body and employs external interventions to optimize the healing process.”
The device features an onboard camera, developed by Associate Professor of ECE Mircea Teodorescu, which captures wound images every two hours. These images are analyzed by a machine learning model referred to as the “AI physician,” developed by Associate Professor of Applied Mathematics Marcella Gomez, which runs on a nearby computer.
“It’s essentially a microscope in a bandage,” Teodorescu stated. “Although individual images may not convey much, continuous imaging enables the AI to detect trends, evaluate wound healing stages, flag complications, and recommend treatments.”
AI-Driven Treatment Administration
The AI physician utilizes the captured images to diagnose the current stage of the wound and compares it against an established timeline for optimal healing. If the AI identifies any delays in the healing process, the machine learning model activates a treatment protocol, which may involve the administration of medication via bioelectronics or the application of an electric field to enhance cell migration towards wound closure.
The medication delivered through the device is fluoxetine, a selective serotonin reuptake inhibitor that modulates serotonin levels in the wound, thereby reducing inflammation and promoting tissue closure. The dosing, optimized through preclinical studies conducted by the Isseroff group at UC Davis, is administered by bioelectronic actuators designed by Rolandi. Additionally, the electric field, which has been refined in previous research by UC Davis’s Min Zhao and Roslyn Rivkah Isseroff, is integrated into the device.
The AI physician is responsible for determining the ideal dosage of medication and the strength of the applied electric field. Following treatment, the device captures another image, and the iterative assessment process begins anew.
During operation, the device transmits images and relevant data, such as the healing rate, to a secure web interface, allowing a human physician to monitor and manually adjust the treatment as necessary. The device conveniently attaches to commercially available bandages for ease of use.
Clinical Testing and Efficacy
To evaluate its clinical applicability, the UC Davis team conducted tests using preclinical wound models. Results from these studies revealed that wounds treated with “a-Heal” exhibited a healing trajectory approximately 25% faster than standard care. These promising findings not only highlight the device’s potential for accelerating the healing of acute wounds but also for revitalizing stalled healing in chronic cases.
AI Reinforcement Learning
The AI system employs a reinforcement learning strategy, as described in a study published in the journal Bioengineering, to replicate the diagnostic methods utilized by physicians. In this approach, the model is designed to achieve the objective of minimizing the time to wound closure, receiving rewards for progressively reaching that goal.
The reinforcement learning model is driven by an algorithm, named Deep Mapper and developed by Gomez and her team. This algorithm processes wound images to quantify the healing stage relative to normal healing timelines, effectively mapping the trajectory of healing. As the device remains attached to the wound, it learns from past healing data and forecasts future healing trends.
As Gomez noted, “It’s not sufficient to merely capture the image; the data must be processed and contextualized to enable feedback control.”
This technique allows the algorithm to learn in real-time about the effects of the medication and electric field on healing, guiding the reinforcement learning model’s iterative decision-making in adjusting the drug dosage or electric-field intensity.
The research team is currently investigating the device’s potential for enhancing the healing of chronic and infected wounds.
This research received support from the Defense Advanced Research Projects Agency as well as the Advanced Research Projects Agency for Health.
Key Health Takeaway
The “a-Heal” device represents a significant advancement in wound care, leveraging AI to personalize treatment and expedite the healing process, with potential applications in both acute and chronic wound management.