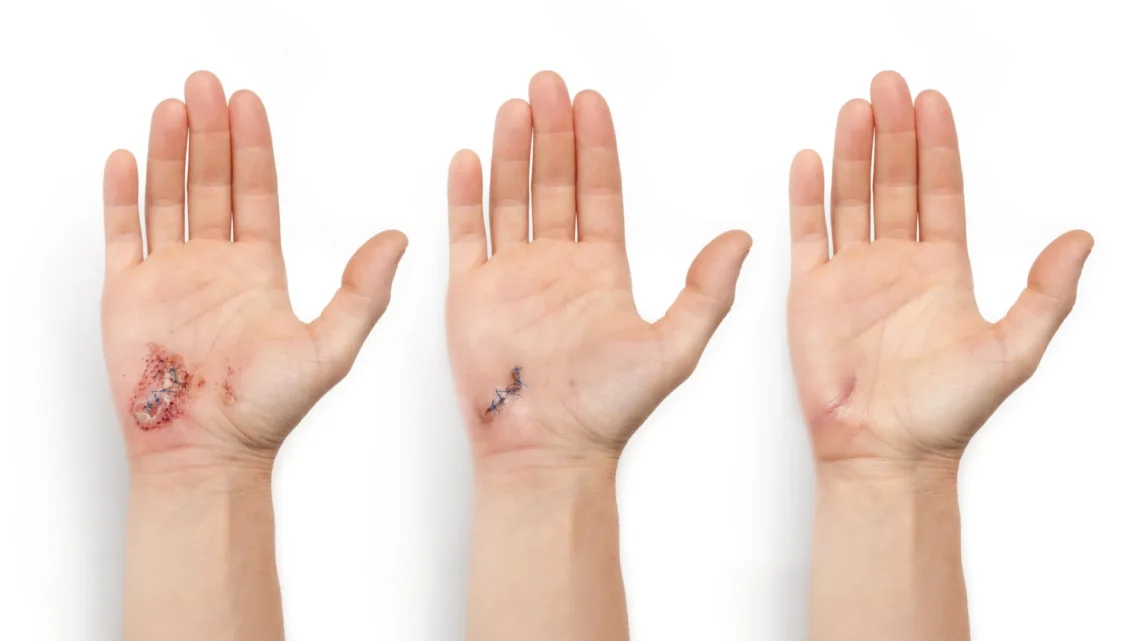
Understanding Wound Healing Stages
Wound healing encompasses several sequential stages, including clotting to prevent bleeding, the immune response, scabbing formation, and ultimately, scarring.
Innovative Technology: a-Heal
A groundbreaking wearable device, named “a-Heal,” has been developed by engineers at the University of California, Santa Cruz. This system aims to optimize each stage of the wound healing process by utilizing a tiny camera and artificial intelligence (AI). The device is capable of detecting the current healing stage and administering appropriate treatments, including medication or an electric field, tailored to the individual patient’s healing requirements.
The portable and wireless design of a-Heal could enhance accessibility to wound therapy, particularly for patients in remote areas or those with limited mobility. Preliminary preclinical results, published in the journal npj Biomedical Innovations, indicate that the device significantly accelerates the healing process.
Design and Functionality of a-Heal
A team of researchers from UC Santa Cruz and UC Davis, sponsored by the DARPA-BETR program and led by Professor Marco Rolandi, has successfully integrated a camera, bioelectronics, and AI into this innovative device. This combination results in a “closed-loop system,” marking one of the first advancements of its kind in the realm of wound healing.
“Our system takes cues from the body and utilizes external interventions to optimize the healing process,” stated Rolandi.
Equipped with an onboard camera, developed by Associate Professor Mircea Teodorescu, the device captures images of the wound every two hours. These images are processed by a machine learning (ML) model, referred to as the “AI physician,” developed by Associate Professor Marcella Gomez, running on a nearby computer.
“Essentially, it’s a microscope embedded within a bandage,” Teodorescu explained. “While individual images provide limited insight, ongoing imaging enables the AI to identify trends, monitor healing stages, detect potential issues, and propose treatments.”
AI-Driven Diagnosis and Treatment
The AI physician analyzes the captured images to diagnose the current wound stage and assesses it against an established timeline for optimal healing. Should the images indicate a delay in healing, the ML model implements one of two treatments: medication delivered via bioelectronics or an electric field designed to enhance cellular migration towards wound closure.
The medication utilized is fluoxetine, a selective serotonin reuptake inhibitor that modulates serotonin levels at the wound site, promoting healing by reducing inflammation and facilitating tissue closure. The optimal dosage, established through preclinical studies conducted by the Isseroff group at UC Davis, is administered by bioelectronic actuators developed by Rolandi. Additionally, an electric field, previously optimized by researchers at UC Davis, is applied through the device.
The system determines the ideal medication dosage and electric field strength. After treatment, the camera captures another image, and this feedback loop continues, enhancing the rehabilitation process.
During operation, the device transmits images and relevant healing data to a secure web interface, allowing healthcare providers to manually adjust treatments as necessary. The device is conveniently attached to a commercially available bandage for ease of use.
Clinical Potential and Results
To evaluate clinical viability, the UC Davis research team conducted tests using preclinical wound models. Results showed that wounds treated with a-Heal displayed a healing trajectory approximately 25% faster than conventional care methods. This underscores the technology’s potential not only for expediting acute wound closure but also for revitalizing the healing of chronic, stalled wounds.
Reinforcement Learning in AI
The AI utilized in the a-Heal device employs a reinforcement learning approach, designed to simulate the diagnostic methods used by healthcare professionals. Reinforcement learning models are structured to achieve specific goals through trial and error, in this case, minimizing the time required for wound closure. The model learns from each patient and adjusts treatment strategies accordingly.
This adaptive learning is facilitated by an algorithm, termed Deep Mapper, created by Gomez and her team. This algorithm processes wound images to determine the healing stage relative to normal healing progressions, which helps project the future healing trajectory.
“It is essential not only to capture the images but also to interpret those images contextually, allowing for effective feedback control,” Gomez emphasized.
This methodology enables the algorithm to evaluate in real-time how the medication or electric field influences healing and directs the reinforcement learning model in making iterative decisions regarding drug concentration or electric field intensity.
The research team is currently exploring the device’s potential to enhance the healing of chronic and infected wounds. For additional publications related to this work, refer to the provided links.
This research has been supported by the Defense Advanced Research Projects Agency (DARPA) and the Advanced Research Projects Agency for Health (ARPA-H).
Key Health Takeaway
The a-Heal device represents a significant advancement in personalized wound care, utilizing AI and bioelectronics to tailor treatments based on individual healing processes, thereby promoting faster recovery for both acute and chronic wounds.